Healthcare professionals, including veterinarians, have been facing increasing vaccine hesitancy rates since the COVID pandemic. This stems from the all-too-real-misconceptions, misinformation, and disinformation disseminated throughout the pandemic.
Sadly, due to this human vaccine hesitancy, we see a spillover into veterinary medicine. Those who are more likely to hesitate to get vaccinations for themselves or family members are more likely to hesitate before giving a dog or cat needed vaccinations.1
So, what does this mean for the veterinary profession as a whole? First, it demonstrates human and animal health are intertwined, and people’s attitudes and beliefs impact their choices about their health and that of their pets. Vaccine hesitancy is a One Health concern.
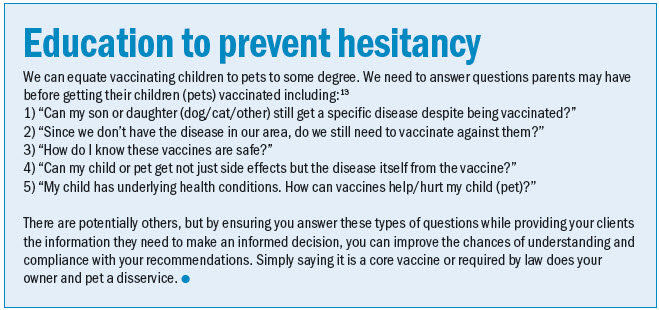
Secondly, vaccine hesitancy requires veterinarians to return to the basics of pet parent education. We may be forced to explain to owners what the diseases we are vaccinating against can do, how contagious they are, and how easily they can be obtained from the environment.
This illustrates the interconnectedness of vaccinations within the One Health framework and their significance in promoting public health, encompassing herd health, human health, and the well-being of individual animals (e.g., in daycare, grooming, or boarding facilities). Though vaccine hesitancy is concerning, it emphasizes effectively communicating to owners the economic value and health benefits of preventive medicine.
What is vaccine hesitancy?
Simply put, vaccine hesitancy refers to when one hesitates or declines to vaccinate (themselves or a pet); cost concerns aside, it is most commonly associated with apprehensions (real or imagined) about the safety and efficacy of a vaccine(s).2,3 Further, this hesitancy is considered by the World Health Organization (WHO) to be one of the world’s top 10 global public health threats.4,5
We do not need to contribute to increasing disease states by undervaccinating pets, but how can we get around this hesitancy? First and foremost, client education is paramount. Helping clients understand the benefits of protecting individual animals and, by extension, those with whom a pet interacts, saves lives and money. Overcoming hesitation is easiest when it involves legally mandated vaccinations, namely rabies. Trouble arises with core and non-core vaccinations without that legal push.
Lacking herd immunity
One concern with vaccine hesitancy arises when insufficient numbers are vaccinated to achieve collective or herd immunity.4,6 Failing to vaccinate one individual animal can have negative impacts on that single animal and its family. However, as we all know, looking at the bigger picture through a One Health lens, failing to vaccinate one then two leads to fewer overall individuals vaccinated and threatens the protective capability of vaccines for an entire population.
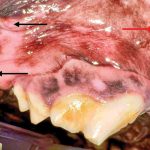
Undervaccination may have spillover effects to other species depending on the disease of concern. Compare the similarity between COVID-19 vaccine hesitancy and the numbers of species capable of both contraction and clinical disease and distemper, which is very contagious to canine species (wild and domestic), ferrets, rodents, tigers (endangered), and several marine mammals, among other species.7–9 This helps demonstrate yet another clear reason why ensuring our pets are vaccinated helps global health prevention.
Why people hesitate
Despite the advent of immunizations being one of modern society’s greatest public health innovations,10,11 people still hesitate to follow vaccination recommendations, even those with high-grade evidence of efficacy and safety.
Reasons for human vaccination hesitancy (that, in turn, impacts pet vaccination rates) include:3,12,13
- Overall concerns about safety
- Side effects
- Misinformation
- Distrust of various entities from the government to healthcare professionals, scientists, and drug companies
- Recognizing trusted resources
- Fear of needles (which, in turn, could be imparted to veterinary patients: owners fearing that their pets are hurting, hate the vet, etc.)
- Inconsistent, even incomplete, recommendations by professionals
Additional reasons for resisting vaccinations include religious beliefs, trypanophobia (fear of needles), a perception (real or imagined) the vaccine is worse than the disease, and cost. Further, accessibility and inequities in human healthcare affect many people’s decisions. Political concerns and failure to comprehend how vaccines work also negatively impact vaccine uptake.
Many people feel vaccines guarantee they will not get sick. They see people vaccinated ill and figure the vaccine does not work.
Educating people that we cannot prevent all infections, but, hopefully, can prevent individuals from getting sick, being hospitalized, or dying, is crucial. Many fail to understand the difference between infection and illness.3,12,13
Still, regardless of the reason people elect not to get vaccinated, those who are less inclined, according to a 2023 survey of 200 Americans, are less likely to vaccinate their dogs. Another survey assessed Americans and Canadians and found regions with anti-vax movements had higher rates of vaccine hesitancy for dogs and cats.2,14
Empowering rabies vaccination
Rabies vaccination is required in most states by law for dogs and cats (though the definition of those needing to be vaccinated, the age of vaccination, and the frequency of vaccination will vary).
While saying people need to have their pets vaccinated because it is the law may achieve the goal of getting the pet vaccinated the day it is in your hospital, it does not fully educate them about the benefits and reasons. Thus, veterinary professionals must explain to clients the disease is almost universally fatal, with up to 60,000 annual deaths globally.15 We should inform them that because of a successful vaccination campaign in our domestic dogs, we successfully rid the U.S. of endemic (wild strain) canine rabies virus.
However, this may spur a question: “So why vaccinate if we do not have canine rabies here?” The answer is easy and twofold. We still vaccinate against rabies, first, because there are wildlife variants to which our animals can be exposed, and second, because animals from other countries could and have inadvertently come into the U.S. carrying the virus. Thus, vaccination is the safest and most effective way to prevent infection and death and to prevent a resurgence of the canine variant in the country.

Empowering key infectious disease vaccines
While rabies still has the legal compeller, other core and non-core vaccines do not. We must strive to reach owners and ensure they understand the different diseases, how serious they are, how easily transmitted they can be, the environments in which animals are exposed, and other pertinent information.
Discuss with clients key factors that play a role in our decision-making process, such as whether we recommend a vaccine or not. Gone (hopefully) are the days when vaccinations were used as the drawing factor to bring animals into one’s practice. Though vaccines still make up a huge part of routine preventive care, we want to emphasize it is not about getting patients into our offices. It is about the benefits of preventive vs. reactive treatment once signs develop, de-emphasizing the importance of vaccination to a practice’s bottom line.
We should recommend core vaccinations for all healthy pets (dogs/cats) without contraindications. However, we may encourage increased intervals between vaccinations as pets age. Further, we want to consider various factors for non-core vaccinations in determining which we recommend for what patient. These factors include:1
- A pet’s overall health status (underlying conditions, medications)
- A pet’s age (young and old; vaccine approval age; legal requirements)
- Prior vaccination history (just a booster, or is a series needed)
- Any previous vaccine reactions (severity of reaction; is premedication required; spacing out vaccinations and giving only one per visit)
- Environmental risks
- Vector exposure
- Exposure to other animals, including daycare, boarding, grooming, recreation, sporting activities, shows, and exposure to other species
Use personal anecdotes or opinions to help guide owners. We have all been asked the dreaded question, “What would you do if it were your pet?” In the case of vaccinations, that is a no-brainer. We vaccinate. We know and trust the scientific evidence (high-grade), and in accordance with our veterinary oath, pledge to do no harm or minimize it, which vaccines greatly assist in. Consider using the American Animal Hospital Association (AAHA) Vaccination Recommendation Schedule,16 which helps guide selections based on various factors, as mentioned above.
Be an active listener
Ensure you spend some of your time listening and not just educating. Ensure you recognize where a client is coming from when declining or hesitating to accept a vaccination recommendation. Beliefs, emotions, and circumstances (economic and otherwise) help to explain why owners hesitate to vaccinate. Be understanding and reassuring to owners at all times. Practice active listening and reflect back that you are hearing them. No matter what you say, some people will not readily vaccinate their pets. But you have done your job and due diligence by educating and imparting your knowledge.
Be proactive
Some owners may simply not like to see their pets suffer. Though expected, perhaps the last time, the pet had a “reaction,” thus, they will hesitate to get future vaccinations. Address any concerns of pain upfront. Offer to provide pain medication if owners feel pets are in pain after vaccines. Discuss how when people are vaccinated, they may be sore in the area for a few days, have a headache, or feel general malaise. Our pets are no different, except they cannot always verbalize it to us in a way we fully understand.
Ensure owners are comfortable knowing they can reach out for meds or advice if they feel the pet is in pain. If a pet previously had a reaction (not allergic, but it was very painful, not eating well for a few days), send Fluffy home proactively with pain meds. This shows owners you are listening and caring for their pets ahead of the game.

Acceptance is key to prevention
We need the help of our pet parents to fully advocate for our patients. Without someone giving us permission to vaccinate, we have no authority. We need our owners, herd managers, farmers, and related individuals to understand why we vaccinate, and we have evidence to support the science. We are not using vaccines that are just off the market and have never been used or studied. Unlike the COVID vaccines that initially utilized Emergency Use Authorization (EUA), we use fully licensed vaccinations with established studies and research demonstrating effectiveness and overall safety.
We must strive to minimize vaccine hesitancy. By properly educating clients, informing them of the benefits of vaccination, key information about the diseases vaccines help to prevent, the improved quality of life, and overall improvements in length of life, we can help them to choose wisely. We want pet and pet parents to have a long, healthy human-animal bond. Preventive medicine and vaccinations are key in maintaining and strengthening this bond.
Erica Tramuta-Drobnis, VMD, MPH, CPH, is the CEO and founder of ELTD One Health Consulting, LLC. Dr. Tramuta-Drobnis works as a public health professional, emergency veterinarian, freelance writer, consultant, and researcher. She is passionate about One Health issues and believes pet health, food safety, agricultural health, and more can address the interconnection of human, animal, and environmental health.
References
- American Veterinary Medical Association (AVMA). Vaccine hesitancy gives some .S.U.S. dog, cat owners cold feet. AVMA (American Veterinary Medical Association). Published January 23, 2024. Accessed March 4, 2024.
- Motta M, Motta G, Stecula D. Sick as a dog? The prevalence, politicization, and health policy consequences of canine vaccine hesitancy (CVH). Vaccine. 2023;41(41):5946-5950. doi:10.1016/j.vaccine.2023.08.059
- Leigh JP, Moss SJ, White TM, et al. Factors affecting COVID-19 vaccine hesitancy among healthcare providers in 23 countries. Vaccine. 2022;40(31):4081-4089. doi:10.1016/j.vaccine.2022.04.097
- Bussink-Voorend D, Hautvast JLA, Vandeberg L, Visser O, Hulscher MEJL. A systematic literature review to clarify the concept of vaccine hesitancy. Nat Hum Behav. 2022;6(12):1634-1648. doi:10.1038/s41562-022-01431-6
- World Health Organization (WHO). Ten Threats to Global Health in 2019. World Health Organization. Published 2019. Accessed March 5, 2024.
- American Veterinary Medical Association (AVMA). Vaccine hesitancy. American Veterinary Medical Association (AVMA). Published February 12, 2020. Accessed March 5, 2024.
- Martinez-Gutierrez M, Ruiz-Saenz J. Diversity of susceptible hosts in canine distemper virus infection: a systematic review and data synthesis. BMC Veterinary Research. 2016;12(1):78. doi:10.1186/s12917-016-0702-z
- Cornell K. Lisa Yang Center for Wildlife Health. Canine Distemper Virus and Tigers | Cornell K. Lisa Yang Center for Wildlife Health | Cornell University. Cornell University. Accessed March 5, 2024.
- Fitzgerald SD, Melotti JR, Cooley TM, Wise AG, Maes RK, O’Brien DJ. GEOGRAPHIC SPREAD OF CANINE DISTEMPER IN WILD CARNIVORES IN MICHIGAN, USA: PATHOLOGY AND EPIDEMIOLOGY, 2008–18. Journal of Wildlife Diseases. 2022;58(3):562-574. doi:10.7589/JWD-D-21-00184
- Centers for Disease Control & Prevention (CDC). Ten Great Public Health Achievements — United States, 2001–2010. Centers for Disease Control and Prevention. Published May 20, 2011. Accessed March 4, 2024.
- Ten Great Public Health Achievements—Worldwide, 2001-2010. JAMA. 2011;306(5):484-487.
- Freeman D, Lambe S, Yu LM, et al. Injection fears and COVID-19 vaccine hesitancy. Psychol Med.:1-11. doi:10.1017/S0033291721002609
- Shen S (Cindy), Dubey V. Addressing vaccine hesitancy. Can Fam Physician. 2019;65(3):175-181. Accessed March 4, 2024.
- Kogan LR, Hellyer PW, Rishniw M. American and Canadian veterinarians’ perceptions on dog and cat core vaccination rates and the impact of the human medicine anti-vaxx movement on veterinary medicine. The Canadian Veterinary Journal. 2021;62(3):247. Accessed March 4, 2024.
- Centers for Disease Control & Prevention (CDC). Rabies around the World – Rabies. Centers for Disease Control and Prevention. Published July 29, 2020. Accessed March 5, 2024.
- AAHA (American Animal Hospital Association). Vaccine Recommendation Schedule Based on Age at Initial Vaccination and Lifestyle of Dog. AAHA. Accessed March 5, 2024.